The term “broken back” conjures images of a dramatic spinal snap, but the reality is often less dire – and much more treatable. While it can be incredibly painful and limiting, a “broken back” typically refers to a fractured vertebra, not a complete spinal cord tear.
A traditional adult spine contains 24 vertebrae, and a fracture usually involves a single vertebra collapsing. This, known as a vertebral compression fracture, is a surprisingly common occurrence. While these fractures are the most common in those with osteoporosis, even those with the healthiest bones can succumb to a compression fracture from a car accident, sports mishap, or a nasty fall. In fact, these fractures affect roughly 1.5 million Americans annually, with older individuals being the most susceptible.
The good news: vertebral compression fractures often bypass the operating room! Most cases can be effectively managed without surgery in an office setting.
But how am I even meant to know that I have a Vertebral Compression Fracture?
 Not all breaks are dramatic. While traumatic accidents are a common culprit for fractures, for those with advanced osteoporosis, even seemingly ordinary actions can wreak havoc. Sneezing a little too hard, stepping out of the shower, or lifting a grocery bag – all have the potential to trigger a fracture. The mundane nature of the cause can leave you bewildered by the sudden, debilitating pain.
Not all breaks are dramatic. While traumatic accidents are a common culprit for fractures, for those with advanced osteoporosis, even seemingly ordinary actions can wreak havoc. Sneezing a little too hard, stepping out of the shower, or lifting a grocery bag – all have the potential to trigger a fracture. The mundane nature of the cause can leave you bewildered by the sudden, debilitating pain.
To determine whether you have a vertebral compression fracture, your doctor will likely ask you some questions.
- Did the back pain appear abruptly, without warning?
- Does standing or walking intensify the discomfort?
- Does lying down increase your pain?
- Is your back pain significantly limiting your mobility?
If these questions all point towards yes, you might have a vertebral compression fracture.
Diagnosis: A Piece of the Puzzle
Before jumping into treatment, your doctor will conduct a physical exam and analyze X-rays or other scans. This “detective work” helps pinpoint the fractured vertebra, estimate the fracture’s age, and determine if kyphoplasty is the most suitable solution. It’s important to note that kyphoplasty isn’t a one-size-fits-all solution for vertebral fractures. It’s most effective for recent fractures and isn’t typically considered for stress fractures as bracing has been found to be effective in many of these cases.
From Broken to Braced: The Kyphoplasty Fix for Back Pain

If Kyphoplasty is seen as the best treatment option, it can be performed as an outpatient procedure right here in our office! Local anesthesia is used to numb the area and our experienced team will be there to help keep your calm, comfortable, and relaxed. We understand that you might feel nervous about being awake during such a procedure, but we assure you that pain is minimal. However, the tools used might generate some unfamiliar noises that can be bothersome. This is why we recommend bringing your favorite tunes and wearing headphones to help distract you during the procedure.
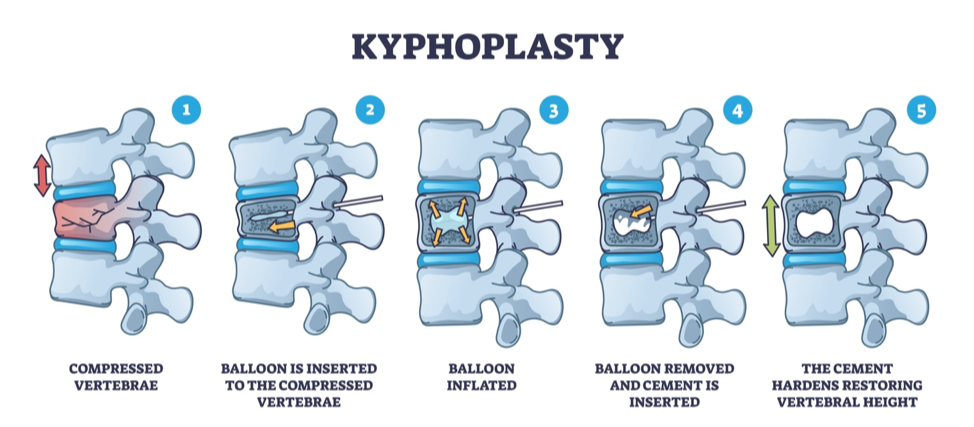
Once your back is comfortably numb, we’ll use a special X-ray device called a fluoroscope as our guide. With its help, we’ll insert a thin, hollow needle into the fractured vertebra. Next comes a tiny balloon that travels through the needle and inflates gently within the vertebral body. This inflation helps nudge the vertebra as close to a pre-fracture position as possible. Once vertebral position is restored, the balloon gets deflated and removed, leaving a small cavity in its wake.
With the same needle in place, we’ll inject liquid bone cement into the cavity created by the balloon. As this cement hardens, it acts like a stabilizer, supporting the fractured vertebra and preventing further movement. Once the procedure is complete, the needle is removed, and the tiny entry point is closed. The whole process typically takes 30-60 minutes, followed by a short rest period on your back to allow the cement to solidify. Typically, patients can experience almost instantaneous improvement of pain and mobility. The bone cement is never removed and becomes a permanent resident inside the vertebra, acting as an internal cast to stabilize it and prevent further issues.
Heads Up: A Word on Potential Hiccups
Let’s be honest, no procedure is entirely risk-free. Kyphoplasty is no exception. There’s a small chance of complications like infection, embolism (a blood clot traveling to another part of your body), leakage of the cement, or even an allergic reaction. The good news? For the vast majority of patients, kyphoplasty is a safe and effective option.
Science Says Kyphoplasty Rocks
Recent years have seen a surge in kyphoplasty research, and the results are music to our ears! Studies consistently show it’s a fantastic treatment option for recent (acute) or subacute (fairly recent) thoracic and lumbar compression fractures.
For example, a 2018 study published in the prestigious International Journal of Spine Surgery concluded that “Overall, Kyphoplasty appears superior in the management of painful compression fractures compared with conservative management.” In other words, kyphoplasty might be a better choice than just taking it easy and hoping for the best.
Let’s Get You On the Road to Recovery
If you’ve been struggling with back pain caused by a compression fracture, kyphoplasty might be the key to getting back to your life. It’s a minimally invasive procedure with a high success rate, offering significant pain relief and improved mobility. While every patient’s journey is unique, our team at Integrative Pain Specialists is here to guide you every step of the way. We can answer your questions, address your concerns, and help you determine if kyphoplasty is the right option for you. Don’t hesitate to contact us today – let’s get you back on the road to recovery!

